In the quest to understand type 2 diabetes (T2D), scientists are delving into the microscopic world of our gut bacteria. Recent research has uncovered intriguing connections between these tiny organisms and the effectiveness of incretin hormones, which are crucial for regulating blood sugar levels. Let's explore how specific gut bacteria might be playing a significant role in T2D and what this means for treatments involving GLP-1 medications.
Incretin hormones, such as GLP-1 (Glucagon-Like Peptide-1) and GIP (Glucose-Dependent Insulinotropic Polypeptide), are essential for stimulating insulin secretion in response to meals. However, these hormones are rapidly broken down by an enzyme called Dipeptidyl Peptidase-4 (DPP4), resulting in their short-lived action [oai_citation:1,PDB-101: Molecule of the Month: Dipeptidyl Peptidase 4](https://pdb101.rcsb.org/motm/202) [oai_citation:2,DPP-4: The Physiology of Incretin Degradation - Progress in Type 2 Diabetes Care](https://www.medpagetoday.com/resource-centers/progress-in-type-2-diabetes-care/dpp/6).
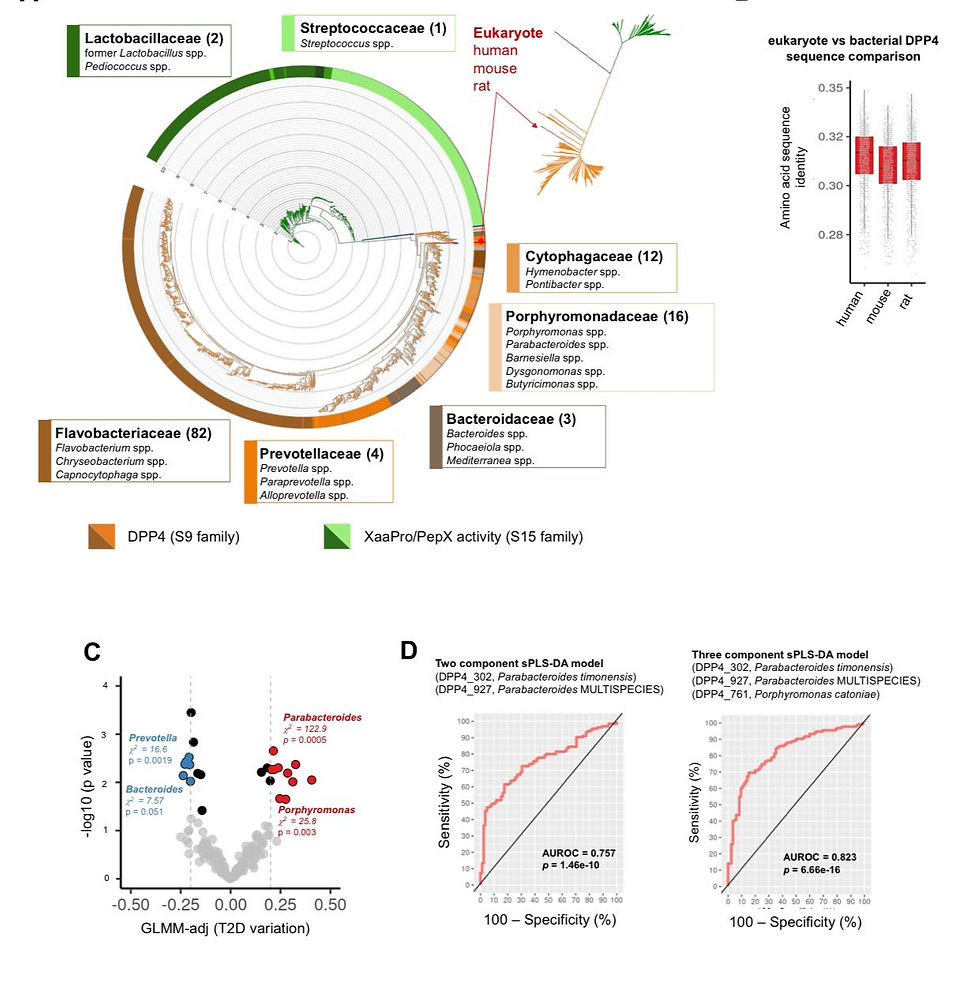
Emerging studies have highlighted that the composition of our gut microbiome can significantly affect DPP4 activity. Individuals with T2D often have higher levels of bacteria that produce DPP4-like enzymes. These bacteria, including species from the Porphyromonadaceae, Flavobacteriaceae, Prevotellaceae, and Bacteroidaceae families, enhance the degradation of incretin hormones, making them less effective at controlling blood sugar levels [oai_citation:3,IJMS | Free Full-Text | Comparative Binding Study of Gliptins to Bacterial DPP4-like Enzymes for the Treatment of Type 2 Diabetes Mellitus (T2DM)](https://www.mdpi.com/1422-0067/25/11/5744) [oai_citation:4,Study finds link between gut microbes and Type 2 diabetes — Harvard Gazette](https://news.harvard.edu/gazette/story/2021/01/study-finds-link-between-gut-microbes-and-obesity/).
Key Research Findings
1. Bacterial Impact on DPP4 Production:
Research indicates that certain bacterial families in the gut microbiome of T2D patients are associated with increased DPP4 production. This leads to a quicker breakdown of incretin hormones, reducing their efficacy in blood sugar regulation [oai_citation:5,A metagenome-wide association study of gut microbiota in type 2 diabetes | Nature](https://www.nature.com/articles/nature11450.pdf) [oai_citation:6,Gut Bacteria May Play a Role in Diabetes](https://www.cedars-sinai.org/newsroom/gut-bacteria-may-play-a-role-in-diabetes/).
2. Predictive Models Using Gut Bacteria:
Scientists have developed models showing that the presence of specific DPP4-producing bacteria can predict the likelihood of developing T2D. These models suggest that higher levels of these bacteria correlate with an increased risk of poor blood sugar control [oai_citation:7,IJMS | Free Full-Text | Comparative Binding Study of Gliptins to Bacterial DPP4-like Enzymes for the Treatment of Type 2 Diabetes Mellitus (T2DM)](https://www.mdpi.com/1422-0067/25/11/5744).
3. Diet and Microbiome Composition:
A study by Andrew T. Chan from Harvard-affiliated Massachusetts General Hospital found that diets rich in healthy, plant-based foods were linked to beneficial gut bacteria that could lower the risk of T2D. This underscores the potential for dietary interventions to modulate the microbiome and improve metabolic health [oai_citation:8,Study finds link between gut microbes and Type 2 diabetes — Harvard Gazette](https://news.harvard.edu/gazette/story/2021/01/study-finds-link-between-gut-microbes-and-obesity/).
Understanding the interplay between gut bacteria and DPP4 activity offers new avenues for personalized medicine in T2D management. Current treatments that inhibit DPP4, such as gliptins, are already in use. However, tailoring these treatments based on an individual’s gut bacterial composition could enhance their effectiveness and minimize side effects [oai_citation:9,Dipeptidyl Peptidase-4 (DPP4) Inhibitors | SpringerLink](https://link.springer.com/chapter/10.1007/978-3-030-86020-2_27) [oai_citation:10,ENP52: Incretins and Type 2 Diabetes Management | Endocrine Society](https://www.endocrine.org/podcast/enp52-incretins-and-type-2-diabetes-management).
Moreover, this research could explain why some patients, often referred to as “slower responders,” do not experience immediate benefits from GLP-1 medications. These medications, which act as metabolic modulators, help to compensate for gut hormonal dysregulation by boosting the levels of incretin hormones. In individuals with higher levels of DPP4-producing bacteria, the incretins are broken down more rapidly, reducing the medication's effectiveness initially. Over time, as these medications modulate the gut environment and hormone levels stabilize, patients may begin to see improvements [oai_citation:11,PDB-101: Molecule of the Month: Dipeptidyl Peptidase 4](https://pdb101.rcsb.org/motm/202) [oai_citation:12,DPP-4: The Physiology of Incretin Degradation - Progress in Type 2 Diabetes Care](https://www.medpagetoday.com/resource-centers/progress-in-type-2-diabetes-care/dpp/6) [oai_citation:13,ENP52: Incretins and Type 2 Diabetes Management | Endocrine Society](https://www.endocrine.org/podcast/enp52-incretins-and-type-2-diabetes-management).
Potential Resolutions
To address the issue of DPP4-mediated degradation of incretin hormones, several strategies are being explored:
1. Personalized Probiotic Treatments: Developing probiotics that specifically target and reduce the population of DPP4-producing bacteria in the gut could help. By rebalancing the gut microbiome, these probiotics might improve the effectiveness of incretin-based therapies.
2. Dietary Interventions: Adopting a diet rich in plant-based foods and low in processed sugars and fats can promote a healthier gut microbiome. Such dietary changes could reduce the prevalence of harmful bacteria and support beneficial ones, enhancing overall metabolic health.
3. Advanced Medication Formulations: While there is already a class of medications known as DPP4 inhibitors, scientists are also working on new formulations of GLP-1 medications that are more resistant to DPP4 degradation. These advanced therapies could provide more sustained blood sugar control, especially in patients with high levels of DPP4-producing bacteria.
Here are some over the counter remedies that seem to hold some promise in reducing DPP4 levels:
1. Cinnamon:
Known for its potential blood sugar-lowering effects, cinnamon may help improve insulin sensitivity. However, more research is needed to confirm its efficacy in weight loss and blood sugar control .
2. Berberine:
An active compound found in several plants, berberine has shown promise in lowering blood sugar levels and improving insulin sensitivity. Like cinnamon, its effectiveness as a DPP-4 inhibitor is not fully established, and further studies are required .
3. Bitter Melon:
This natural supplement is often used in traditional medicine for diabetes management. It may help lower blood sugar levels, but its exact mechanism and impact on DPP-4 levels need more scientific validation .
4. Probiotics
Probiotics are live microorganisms that, when taken in adequate amounts, confer health benefits to the host, particularly by improving gut health. Research suggests that probiotics can positively influence the gut microbiome, potentially reducing the prevalence of harmful bacteria that produce enzymes like DPP-4. By modulating the gut flora, probiotics may help maintain a healthier balance of bacteria, which could, in turn, support better regulation of incretin hormones such as GLP-1 and GIP. These hormones play a crucial role in managing blood sugar levels, and by enhancing their activity through improved gut health, probiotics might offer a supportive strategy in managing type 2 diabetes.
While these supplements might provide some benefits, it’s crucial to consult with a healthcare professional before incorporating them into your regimen, especially if you are managing diabetes. They can help determine the best approach and ensure these supplements do not interfere with any current medications.
The connection between gut bacteria and T2D highlights the importance of considering the microbiome in diabetes treatment and management. As research continues, we may see more personalized approaches to diet and medication that account for an individual’s unique microbiome. Staying informed about these developments can provide new strategies for optimizing health. Always consult with healthcare professionals before making any changes to your treatment plan.
For more insights and updates on managing type 2 diabetes, visit [onthepen.com](http://onthepen.com) and follow @manonthemounjaro for the latest news and personal stories from the journey towards better health.
Sources:
1. [MDPI - Comparative Binding Study of Gliptins to Bacterial DPP4-like Enzymes](https://www.mdpi.com)
2. [Nature - A Metagenome-wide Association Study of Gut Microbiota in Type 2 Diabetes](https://www.nature.com)
3. [Harvard Gazette - Study Finds Link Between Gut Microbes and Type 2 Diabetes](https://news.harvard.edu)
4. [Cedars-Sinai - Gut Bacteria May Play a Role in Diabetes](https://www.cedars-sinai.org)
Feel free to share your thoughts and experiences in the comments below! Let’s continue this journey together!

Comments